Antibiotics target a range of bacteria—both good and bad—to combat bacterial infections. They’re one of the modern marvels of the 21st century, but can they weaken your immune system?
Although antibiotics might seem like a miracle-cure-all drug, they aren’t. Research has shown that improper use of antibiotics can be harmful to your health.
In one study, antibiotics were shown to adversely impact the good bacteria in our digestive system that play a crucial role as our first line of defense against certain infections.
What's the Risk?
If you take antibiotics too often, there is also an increased risk of antibiotic resistance. Antibiotic resistance is when bacteria and viruses learn to defend themselves against antibiotics, making the antibiotics ineffective.

Keep in mind all bacterial infections have the potential to become life-threatening if left unattended. But will taking antibiotics every day keep you immune? Will it harm you in any way?
Here, we’ll explain the different effects of antibiotics and why you should always take them as prescribed.
The Age of Antibiotics
In 1929, Nicolas Fleming published his discovery of penicillin in the 1929 British Journal of Pathology. It wasn't until World War II that a pair of scientists, Howard Florey and Ernest Chain, were able to isolate the medicine for mass production. This paved the way for the scientific research of antibiotics.
All medicines come with potential side effects, from diuretics to ibuprofen. Just because a medication has side effects for some people doesn’t mean it’s dangerous, but you should always pay attention to how your body reacts to new substances.
Some medications help your body regulate or control complex chemicals. Antibiotics work a bit differently. They target the parts of bacterial cells that cause cell death (or apoptosis, if you’re feeling fancy). White blood cells may also attack these bacterial cells as part of an immune response. Once the antibiotics target this bacteria, they can kill it and prevent it from spreading throughout the body.
Antibiotics Are Time Specific
In the United States, antibiotics are strictly regulated to ensure that the patient only receives the exact amount of medicine they will need to destroy the intended bacterial cells.
Going against your doctor’s instructions, such as taking two tablets instead of one, will increase the drug's concentration. This can eventually lead to toxic levels of the drug that can greatly impact your immune system.
Over the course of weeks or even months, you take this antibiotics for treatment (like tuberculosis). Some bacteria have a slow metabolic rate, so they only absorb a little of the antibiotics each day. It can take months to successfully kill off these slow-to-absorb bacteria. Missing even one day of your prescribed treatment can greatly increase these bacteria’s antibiotic resistance, giving them time to develop defenses against the antibiotic, which is especially common in tuberculosis germs.
Bacterias Can Learn To Be Resistant
Drug-resistant bacteria tend to be more aggressive and challenging to treat, and they are recognized as a growing global crisis. Drug-resistant bacteria can tremendously impact your health and lead to greater side effects. If a drug becomes ineffective during treatment and the bacteria has shown drug resistance, it could become difficult to eradicate that bacteria. This may allow the bacteria to spread throughout your body.
Research shows that antibiotics specifically interact with immune cells. Over time, our immune system produces white blood cells to fight the infection alongside the antibiotic regimen. After a period of time, their ability to fight the infection decreases because they have exhausted their resources. At this point, the patient is rendered immuno-compromised because they don’t have the necessary means to fight the infection independently.
Bacterial resistance is why it is important to follow the instructions your prescribing doctor provides. Taking it less than prescribed means you could end up creating drug-resistant bacteria that can’t be killed by future antibiotics. You can’t be harmed instantly by just taking two pills instead of one, or skipping a day of treatment—instead, this contributes to long-term antibacterial resistance because you're essentially "showing your cards" to bacteria when they aren't actively attacking.
Does Taking Antibiotics Build Up Immunity?
Taking more antibiotics than your prescribed doesn't increase immunity or prevent future infections. Research has shown that early use of antibiotics can lead to decreased protective immunity to infections and increased susceptibility to reinfection. It does so by decreasing the capabilities or “memories'' of our immune cells by constantly exposing them to a threat that is not present.
Not All Bacteria Are Bad
What if I told you that our digestion is dependent on bacteria? From the moment we are born, microbiotic flora lines our digestive tract. It is where our immune system first learned to build resistance to bad germs.
This system of “good” bacteria is responsible for a big part of our immunity and our defense against foreign pathogens. Oral antibiotics can diminish the effectiveness of our gut flora since antibiotics can’t tell good bacteria from bad.
If you have ever felt nauseous after beginning antibiotics, this isn’t much of a surprise. Damaged "good" bacteria can cause this nausea. For some, the nausea will pass, but sometimes it can persist and become intolerable. When nausea is persistent, alternative forms of treatment happen.
Gut flora is not only responsible for maintaining digestion. It also plays a crucial role in nutrient metabolism, drug metabolism, protection of the gut lining, and protection against foreign pathogens. Any disruption to the gut flora can have a profound impact on a person's health, mainly their immune system, as it is responsible for many factors that keep us healthy.
Overuse of Antibiotics Can Weaken Your Immune System
Antibiotics have the potential to save countless lives, but improper use can also damage countless lives. For creation of drug-resistant bacteria or worsening disease to occur, we must strictly follow treatment guidelines.
Following your doctor’s orders improves your health and decreases the risk of a prolonged infection that becomes highly contagious, possibly infecting household members.
Use Antibiotics Only When Prescribed
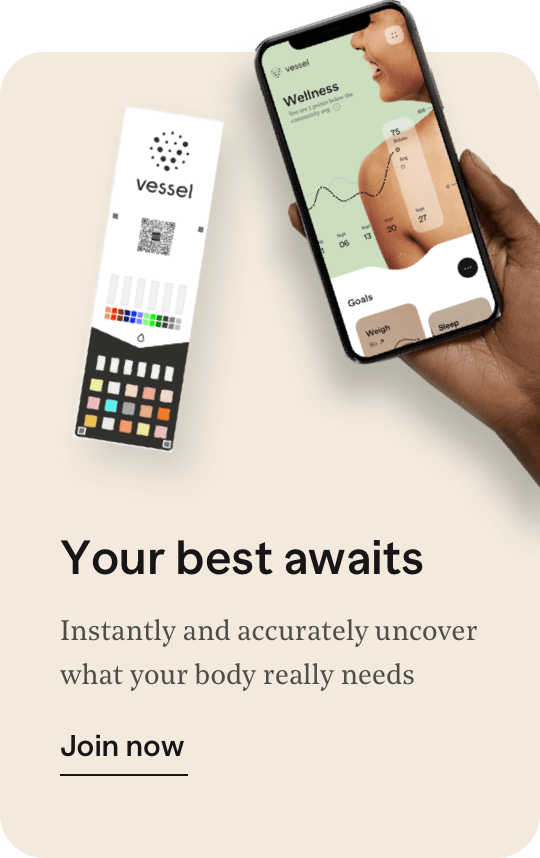
Responsible use of antibiotics is a global call to fight against drug-resistant infections. You should never “self-prescribe” medications—doing so will only do more harm. Antibiotics can help infections that may be fatal, but incorrect antibiotic use can be fatal itself. If you want to learn more about antibiotics, we have unlimited nutritional coaching alongside our daily lesson plans & activities while you monitor your health metrics using our wellness cards. Sign up with Vessel Health today to connect with a coach!
Written by

Mikaela Frame See all the author’s articles